This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
Short case
Prashanth Reddy Anugu
Hall ticket: 1701006141
A 30 year old female patient, who is a housewife and resident of Nalgonda came to OPD with chief complaints of
Facial puffiness for 4 days
Pedal edema for 4 days
Shortness of Breath for 2 days
Abdominal pain for 2 days
History of presenting illness :
Patient was apparently asymptomatic 7 months back. Then she developed facial puffiness (which was insidious in onset, gradual in progression and was observed on waking up in the morning) and Bilateral leg swelling (which was of grade II) .For this the patient consulted the Physician, who after investigating put the patient on certain medications and both the complaints got better.
Now four days back ,she again developed pedal edema of both legs and facial puffiness. Two days ago ,patient developed shortness of breath which was insidious in onset , gradually progressed to grade 4 and was not affected with change in position ,without any aggravating or relieving factors . She also developed abdominal pain 2 days back which was diffuse over the abdomen .
Past history
She is a known case of hypertension for 12 years for which she is on Telmisartan 40 mg
Personal history :
Diet - mixed
Appetite - Decreased
Sleep - Inadequate
Bladder - Decreased urine output
Bowel movements - normal
No addictions.
Family history:
Patient's mother has hypertension.
GENERAL EXAMINATION:
Patient was examined in a supine position in a well lit room after obtaining consent in the presence of a female attendant
Patient was conscious, coherent and cooperative and oriented to time , place and person
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Edema of both the lower limbs below knee
Vitals:
Temperature - Afebrile
Pulse - 110 bpm
Blood pressure - 150/90mmHg
Respiratory rate - 36 cpm
SYSTEMIC EXAMINATION:
ABDOMINAL EXAMINATION
INSPECTION :
Shape - Distended
Umbilicus - normal
Movements - normal
Visible pulsations - absent
Surface of the abdomen - normal
PALPATION :
Liver - Not palpable
Spleen -Not palpable
No fluid thrill
No shifting dullness
AUSCULTATION - Bowel sounds are heard .
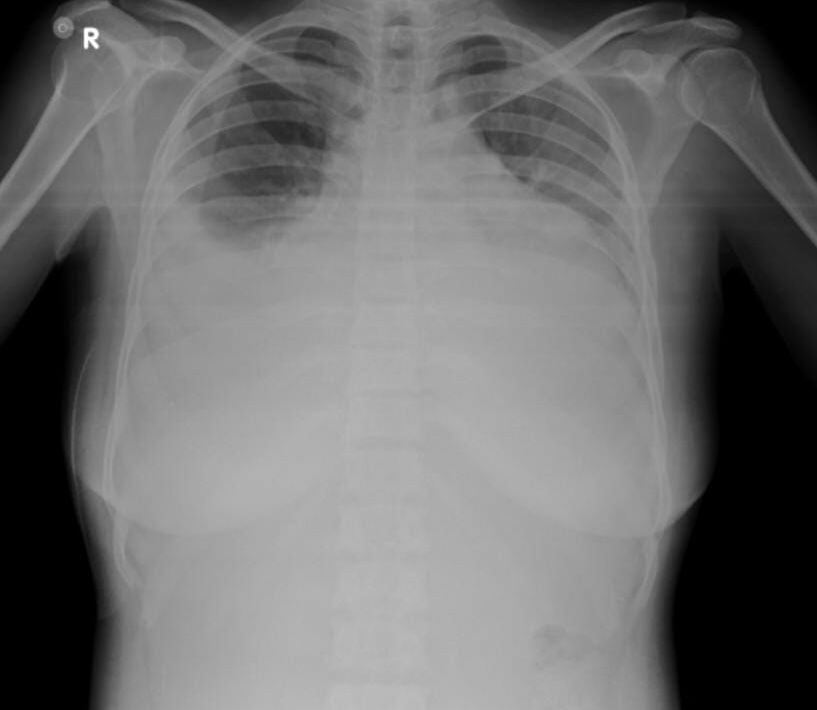
RESPIRATORY SYSTEM EXAMINATION
INSPECTION
Oral cavity- Normal
Nose- normal
Pharynx-normal
Respiratory movements equal on both the sides
Bilaterally symmetrical chest
Trachea - central in position
No scars and sinuses
No engorged veins
No hallowing or flattening of supraclavicular /infraclavicular spaces
Apex impulse visible in 5th intercostal space
PALPATION
No local rise of temperature
No tenderness
All inspiratory findings are confirmed
Trachea - central in position
Apical beat felt in the left 5th Intercoastal space medial to the mid clavicular line
Respiratory movements equal in both the hemithorax
Tactile vocal fremitus - reduced on both sides in infra axillary and infra scapular region
PERCUSSION- Dull on both the sides
AUSCULTATION - Decreased respiratory sounds on both the sides.
CARDIOVASCULAR SYSTEM EXAMINATION
S1, S2 - heart sounds are heard
No audible murmers
NERVOUS SYSTEM EXAMINATION
Motor and sensory systems are intact











Comments
Post a Comment